Introduction
Physical Therapy in Waterbury for Knee Issues
Welcome to Peak Physical Therapy’s resource about Osgood-Schlatter Disease.
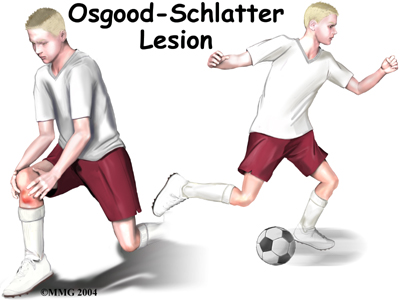
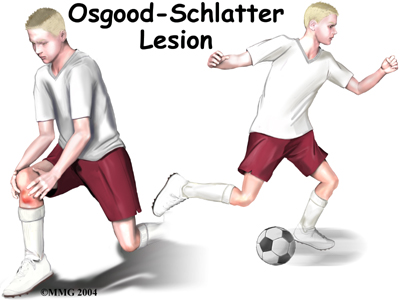 An Osgood-Schlatter lesion involves pain and swelling in the small boney bump on the front of the tibia (shinbone), right below the kneecap. It primarily occurs in children and adolescents. The problem affects the area where bone growth occurs. Too much stress on the growing bone causes the pain and swelling. The pain often worsens with activity and eases with rest. Fortunately, the condition is not serious and it is usually only temporary.
An Osgood-Schlatter lesion involves pain and swelling in the small boney bump on the front of the tibia (shinbone), right below the kneecap. It primarily occurs in children and adolescents. The problem affects the area where bone growth occurs. Too much stress on the growing bone causes the pain and swelling. The pain often worsens with activity and eases with rest. Fortunately, the condition is not serious and it is usually only temporary.
Osgood-Schlatter Disease is the most frequent cause of knee pain in children between the ages of 10 and 15. The problem used to occur mostly in boys but with more girls playing sports, boys and girls are now affected equally. Being that girls' skeletons begin to mature earlier than boys, girls tend to have this condition when they are one to two years younger than boys. Kids who play sports have this condition 20 percent more often than non-athletes. In addition, the lesion seems to run in families; when one child is affected, there's a 30 percent chance a sibling will have it, too.
This guide will help you understand:
- why the condition develops
- how health care professionals diagnose the condition
- what treatment options are available
#testimonialslist|kind:all|display:slider|orderby:type|filter_utags_names:Knee Pain|limit:15|heading:Hear from some of our patients who we treated for *Knee Pain*#
Anatomy
What part of the knee is affected?
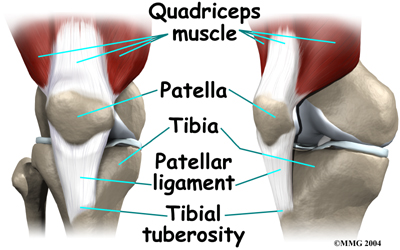
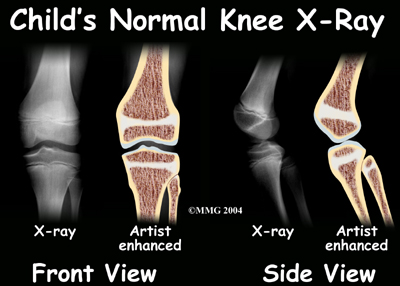
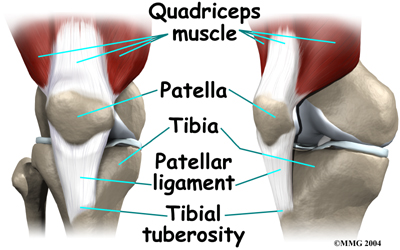
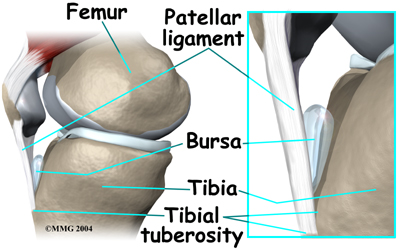
The Osgood-Schlatter lesion affects the tibial tuberosity. The tibial tuberosity is the bump on the top of the tibia (shinbone) where the patellar tendon connects. Tendons connect muscles to bones. The patellar tendon stretches over the top of the patella (kneecap). The patellar tendon connects the large quadriceps muscle on the front of the thigh to the tibial tuberosity. As the quadriceps muscle works, it pulls on the patellar tendon and extends (straightens) the knee joint.
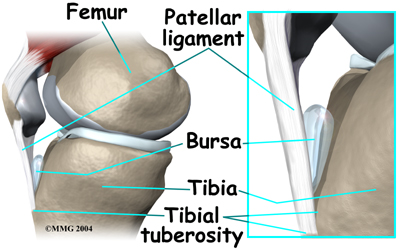
A small bursa sometimes develops where the patellar tendon meets the tibial tuberosity. A bursa is a normal structure that often forms in areas where friction occurs, such as between muscles, tendons, and bones. A bursa is a thin sac of tissue filled with fluid. The fluid lubricates the area and reduces friction. If too much friction occurs, however, the bursa can swell and become a problem itself.
Related Document: Peak Physical Therapy's Guide to Knee Anatomy.
Knee Anatomy Introduction
- Knee
Causes
How did this problem develop?
 Osgood-Schlatter lesions fit into a category of bone development disorders known as osteochondroses. (Osteo means bone, and chondro means cartilage.) In normal development, specialized bone growth centers (called growth plates) change over time from cartilage to bone. The growth centers expand and finally unite. This is how bones grow in length and width. Bone growth centers are located throughout the body.
Osgood-Schlatter lesions fit into a category of bone development disorders known as osteochondroses. (Osteo means bone, and chondro means cartilage.) In normal development, specialized bone growth centers (called growth plates) change over time from cartilage to bone. The growth centers expand and finally unite. This is how bones grow in length and width. Bone growth centers are located throughout the body.
Children with bone development problems in one area are likely to develop similar problems elsewhere. For example, among young athletes with growth plate problems in the back of the heel (Sever’s Syndrome), about two-thirds also develop an Osgood-Schlatter lesion. Children who have an Osgood-Schlatter lesion also have a small chance of problems at the top of the patellar tendon, where it attaches to the bottom tip of the kneecap. This condition is known as Sinding-Larsen-Johansson disorder.
The main cause of Osgood-Schlatter lesions is too much tension in the patellar tendon.
The tension can come from overuse from sports activity and from growth spurts. Usually both happen together and both put extra stress on the tibial tuberosity.
During growth spurts, the tendon may not be able to keep up with the growth of the lower leg and the tendon ends up being relatively too short. The tendon constantly pulls at the tibial tuberosity. Tension from sports activity comes from overuse during the activities. When the quadriceps muscle on the front of the thigh works, it pulls on the patellar tendon. The tendon in turn pulls on the tibial tuberosity. If the tension is too great and occurs too often while the bone is developing, it can pull the growth area of the tibial tuberosity away from the growth area of the shinbone.
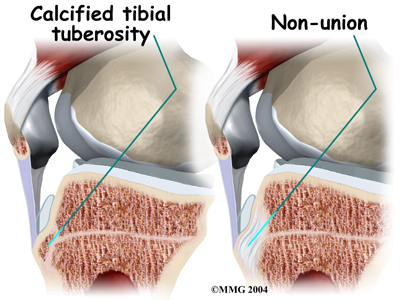
A bump can form at the tibial tuberosity because the separated growth plates keep growing and expanding. The area between the bone fragments fills in with new tissue, either cartilage or bone. The new tissue causes the tibial tuberosity to become enlarged and painful.
Another possible contributing factor to Osgood-Schlatter lesions is abnormal alignment in the legs. Kids who are knock-kneed or flat-footed seem to be prone to developing this condition as these postures form a sharper angle between the thigh bone/quadriceps muscle and the patellar tendon. This angle is called the Q-angle. A large Q-angle puts more tension on the patellar tendon and bone growth plate of the tibial tuberosity, increasing the chances for an Osgood-Schlatter lesion to develop. A high-riding patella, called patella alta, is also thought to contribute to development of Osgood-Schlatter lesions.
Symptoms
What does an Osgood-Schlatter lesion feel like?
 In an Osgood-Schlatter lesion, the tibial tuberosity is often enlarged and painful. It hurts when bumped. It also hurts when pressure is put on it, such as when kneeling. Activities like running, jumping, climbing, and kicking may hurt because of the tension of the patellar tendon pulling on the tibial tuberosity.
In an Osgood-Schlatter lesion, the tibial tuberosity is often enlarged and painful. It hurts when bumped. It also hurts when pressure is put on it, such as when kneeling. Activities like running, jumping, climbing, and kicking may hurt because of the tension of the patellar tendon pulling on the tibial tuberosity.
Symptoms generally go away gradually over a period of one to two years and can be managed in that time with Physical Therapy. The condition, however, may leave a permanent, painless bump below the knee and the area may always be tender when pressure is applied to it. Many adults who had a lesion as a child still have pain when kneeling on that knee.
Complications can occur if the area between the bone fragments fills in with cartilage rather than bone. Normally, the bone growth plates join together with solid bone in between. If cartilage fills in the space, the condition is called a nonunion.
Diagnosis
How do health care professionals diagnose the condition?
Diagnosis begins with a complete history of your child’s knee problem followed by an examination of the knee and related joints. Most often your Physical Therapist at Peak Physical Therapy can make the diagnosis of Osgood Schlatter Disease from the history and physical examination. Your Physical Therapist will ask your child questions about where precisely the pain is, when the pain began, what they were doing when the pain started, and what movements aggravate or ease the pain. They will also inquire about pain elsewhere in the body such as in the hips, heels, or lower back. If your child is active in sport, they will inquire about which sports they are involved in, and how much and how often they are participating. They will also want to know if any siblings have also suffered from knee pain and what the nature of the problem was. The history alone will often lead your Physical Therapist to the suspicion of Osgood Schlatter Disease.
 Next your Physical Therapist will do a physical examination of both your child’s painful and non-painful knee, and examine the entire lower extremities for factors contributing to the problem. Your therapist will palpate, or touch, around the knee and particularly along the patellar tendon and at the tibial tuberosity to determine the exact location of pain and to note any swelling. They will assess the stability of the knee joint to determine if the laxity of the ligaments and tissues surrounding the knee joint are contributing to the problem.
Next your Physical Therapist will do a physical examination of both your child’s painful and non-painful knee, and examine the entire lower extremities for factors contributing to the problem. Your therapist will palpate, or touch, around the knee and particularly along the patellar tendon and at the tibial tuberosity to determine the exact location of pain and to note any swelling. They will assess the stability of the knee joint to determine if the laxity of the ligaments and tissues surrounding the knee joint are contributing to the problem.
In order to assess your child’s individual alignment your Physical Therapist may want to look at how they stand, observe their foot position, or watch them walk, squat, or jump. Your Physical Therapist will also check the strength and lengths (flexibility) of the muscles surrounding and affecting the knee joint such as the quadriceps, hamstrings, calves, hip flexors and buttocks muscles. All of these muscles, if weak or tight, can contribute to an imbalance of forces applied to the knee joint and may contribute to the development of Osgood Schlatter Disease. Providing resistance while your child straightens their knee often reproduces the pain associated with Osgood Schlatter Disease so this will also be tested. Severe weakness during this straightening motion or while squatting on one leg may cause your Physical Therapist to suspect a more serious injury affecting the tibial tuberosity.
Treatment
What can be done for the problem?
Nonsurgical Treatment
Generally the passing of time allows the pain from Osgood-Schlatter Disease to dissipate. It takes one to two years for the bone growth plates of the tibial tuberosity to grow together and form one solid bone. When this occurs, symptoms usually go away completely. As the pain is most often related to the closing of the growth plates, the age of your child when the pain begins can contribute to how long the pain lasts overall.
 Your doctor may prescribe anti-inflammatory medicine to help reduce swelling.
Your doctor may prescribe anti-inflammatory medicine to help reduce swelling.
Working with a Physical Therapist at Peak Physical Therapy can also help to reduce swelling, manage pain levels, aid in activity modification, and assist in developing proper alignment to decrease the stress applied to the painful knee.
Cortisone injections are commonly used to control pain and inflammation in other types of injuries. However, a cortisone injection is usually not appropriate for Osgood-Schlatter lesions. Cortisone injections haven't shown consistently good results for this condition.
There is also a high risk that the cortisone will cause the patellar tendon to rupture.
Rehabilitation
What can be expected from treatment?
Nonsurgical Rehabilitation
With nonsurgical rehabilitation at Peak Physical Therapy, the goal is to reduce pain and inflammation, and decrease the overall stress applied to the knees. Fortunately, most Osgood-Schlatter lesions get better with Physical Therapy treatment and the passing of time as the bones mature. The foremost aim of treatment at Peak Physical Therapy is to decrease the inflammation and pain in the knee. Simply having your child ice their knee can assist with the inflammation and relieve a great deal of the pain. In cases of chronic pain, heat may be more useful in decreasing pain. Your Physical Therapist may also use electrical modalities such as a low-dose ultrasound or interferential current to help decrease the pain and control the amount of inflammation. Massage for the quadriceps, hamstrings, and calf muscles may also be used.
 In some cases, your child may need to stop sporting activities for a short period, which allows the pain and inflammation to calm down. If the bone has completely separated then it is necessary to completely avoid sports. Fortunately it is not common that the bone completely separates, so not all athletes need to entirely avoid sports. Patients who do require a rest usually don't need to avoid sports for a long time, and often a relative rest is adequate. Taking a relative rest means decreasing the intensity or frequency of certain activities but not eliminating them completely. Your Physical Therapist will advise you regarding whether or not your child needs to cease or decrease their activity. Pain that is intense enough to continue during the night, is constant, causes a limp while walking, or needs to be regularly relieved with over the counter pain medication is considered severe enough that activities need to be ceased for a defined period of time. In only very severe cases is bracing or casting recommended for periods of up to 6 weeks in order to give the chance for the pain and inflammation in the knee to calm down.
In some cases, your child may need to stop sporting activities for a short period, which allows the pain and inflammation to calm down. If the bone has completely separated then it is necessary to completely avoid sports. Fortunately it is not common that the bone completely separates, so not all athletes need to entirely avoid sports. Patients who do require a rest usually don't need to avoid sports for a long time, and often a relative rest is adequate. Taking a relative rest means decreasing the intensity or frequency of certain activities but not eliminating them completely. Your Physical Therapist will advise you regarding whether or not your child needs to cease or decrease their activity. Pain that is intense enough to continue during the night, is constant, causes a limp while walking, or needs to be regularly relieved with over the counter pain medication is considered severe enough that activities need to be ceased for a defined period of time. In only very severe cases is bracing or casting recommended for periods of up to 6 weeks in order to give the chance for the pain and inflammation in the knee to calm down.
In some cases your Physical Therapist may try using some tape on your child’s knee. Taping the knee or kneecap can help guide the tissues into an improved alignment, which then relieves some pressure on the painful area at the tibial tuberosity.
Orthotics, or shoe inserts, may also be suggested. The foot is the bottom of the lower extremity chain therefore putting the foot into proper alignment frequently takes pressure off of the knee, and can relief all or some of your child’s pain. Other types of braces, such as those that help to align the knee cap or add padding to the front of the knee can sometimes also be helpfulin reducing the tension and force transmitted to the tibial tubercle. Your Physical Therapist at Peak Physical Therapy can discuss these options with you and your child.
Once the initial pain and inflammation has calmed down, your Physical Therapist will focus on improving the flexibility, strength, and alignment around the knee joint and the entire lower extremity. Static stretches to increase the flexibility of the muscles and tissues affecting the knee (particularly the quadriceps, hamstrings, hip flexors, calf, and iliotibial band on the outside of the knee) will be prescribed by your Physical Therapist early on in your child’s treatment. Any tightness in the muscles or tissues around the knee can increase the pull on the patellar tendon and the tibial tuberosity, which affects alignment during walking, running or jumping. Dynamic stretching (rapid motions that stretch the tissues quickly) will also be taught and will be incorporated into your child’s rehabilitation exercise routine as part of their warm-up if they are continuing to engage in physical activity. Dynamic stretches are used to prepare the tissues for activity whereas static stretches focus more on gaining overall flexibility.
Strength imbalances will also affect the alignment of the knee and can cause muscles to tighten, which in turn may cause increased stress on the patellar tendon and tibial tuberosity. Your Physical Therapist will determine which muscles in your child’s case require the most strengthening. Strength in both the knee and the hip (which controls the knee position) are very important. Increased strength and endurance can affect the ability to maintain one’s alignment, and will directly affect the amount of pressure transferred to the tibial tuberosity. Strengthening a knee that is painful can be difficult therefore it is important to follow the strict instructions of your Physical Therapist regarding increasing or decreasing the load of the exercise. Overdoing an exercise can cause more harm than good in the case of Osgood Schlatter Disease. In some cases your Physical Therapist may use a muscle stimulator on your child’s knee to help recruit the proper muscles around the joint.
Over time, when the knee becomes less painful your therapist will add eccentric exercises to your child’s rehabilitation routine. Eccentric contractions occur as the muscle lengthens and the tendons and their attachment points are put under stretch. For instance, when bending the knee, the quadriceps muscle, the patellar tendon, and its attachment point at the tibial tuberosity are all under load while stretching. This load is tremendous especially when deep squatting, jumping or landing from a jump. Even going down stairs puts significant load through the tissues. Eccentric exercises prepare the tissues to take these heavy types of loads. Exercises that simulate going down stairs or jumping will be prescribed. Drop squats, where your child bends their knee quickly into a squatting position and then stops rapidly, are commonly used to encourage the knee to adapt to the force that is needed to return to physical activity. Again, in dealing with pain from Osgood Schlatter Disease, any discomfort should be strictly heeded. When appropriate, weights can be added to the exercises to simulate the increased body weight that the knee endures during running and jumping. As with all the exercises, proper alignment and technique is extremely important in order to avoid flaring up the knee or creating a secondary injury. Your Physical Therapist will be strict about having your child maintain good technique, and will ask you, as the parent, to also monitor this.
In addition to flexibility and strength exercises your Physical Therapist will also add a proprioceptive, or balance component to your child’s rehabilitation program. With any injury or whenever pain is present, the receptors in your joints that are responsible for knowing where your body is in space decline in function. Without adequate proprioception, the muscles and joints are not used efficiently and the chance of sustaining another injury is increased. Exercises such as mini squats on a soft mat or standing on a wobbly surface are simple exercises that improve proprioception, and will also improve muscle strength and overall endurance.
All exercises given will be required to be completed not only in the clinic but also as part of a home program. Many children and adolescents can reliably do a small list of independent Physical Therapy exercises, however at Peak Physical Therapy we always encourage you, as the parent, to closely monitor the child’s technique and exercise frequency at home in order to get the most out of the treatment we provide.
Peak Physical Therapy provides services for Physical Therapy in Waterbury.
Rehabilitation - Surgery
 Surgery is not considered for an Osgood-Schlatter lesion unless bone growth is complete and symptoms are still bothersome despite nonsurgical treatments. Even under these circumstances, surgery is rarely recommended.
Surgery is not considered for an Osgood-Schlatter lesion unless bone growth is complete and symptoms are still bothersome despite nonsurgical treatments. Even under these circumstances, surgery is rarely recommended.
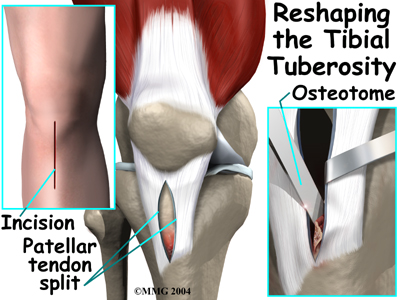
When surgery is needed, however, the usual operation involves removing the raised area of the tibial tuberosity, the bursa, and the irritated tissue nearby. The surgeon makes a small incision down the front of the lower knee, just over the tibial tuberosity. The patellar tendon is split in half. Retractors are used to pull the skin and the patellar tendon apart, which makes it easy for the surgeon to see and work on the tibial tuberosity. The surgeon uses an osteotome to cut away the raised area of the tibial tuberosity. Care is taken while removing the bursa and nearby tissue.
The retractors are removed. The cut edges of the patellar tendon are brought together. Scar tissue eventually binds the edges back together. To complete the operation, the surgeon stitches up the skin.
Post Surgical Rehabilitation
After surgery for Osgood Schlatter Disease rehabilitation at Peak Physical Therapy can begin as soon as your child’s surgeon recommends it. Some surgeons may want your child to rest the knee for a period before doing any rehabilitation while others will be keen to have your child begin gentle rehabilitation almost immediately. When rehabilitation begins depends on the surgeon’s personal experience, the technique used, and other factors specific to your child’s individual case. In every case, however, vigorous activities or exercise will need to be avoided for about six weeks after surgery. Athletes will not be allowed to take part in high-level sports for two to three months.
After surgery your child will likely be required to use crutches for a short period. Your Physical Therapist at Peak Physical Therapy will ensure your child knows how to safely use their crutches both on level ground and on stairs. Your Physical Therapist will advise your child as soon as it is appropriate to walk without the crutches. In order to do this, your child must be able to walk well without any limp at all. Walking with a limp can cause a host of other problems in the joints of the lower extremity and the back so heeding advice from your Physical Therapist on the right timing for your child to go without crutches is imperative.
The first few appointments after surgery at Peak Physical Therapy will focus on helping to control the pain and swelling from the surgery itself. Icing the knee frequently will assist with the inflammation and relieve a great deal of the pain. Your Physical Therapist may use electrical modalities such as low-dose ultrasound or interferential current to decrease the pain and inflammation. Massage for the muscles of the leg or around the knee may
One of the first exercises your child’s Physical Therapist will prescribe will be some gentle range of motion exercises to help the knee to gradually regain full movement. These exercises should be done within a pain free range of motion, however, movement will be encouraged even if it causes a slight bit of discomfort as the movement itself can greatly assist with dispersing any inflammation as well as improving the overall level of pain. A stationary bicycle can be very useful in the initial stages of gaining range of motion in the knee, so if able, your child will be encouraged to use one. Even if they are unable to fully rotate the pedals, the back and forth motion on the bike is an excellent method of slowly encouraging the knee to regain its full range of motion, and to get the swelling moving.
Next your Physical Therapist will begin to add some gentle strengthening exercises for the knee. Initially these may only involve isometric exercises, where your child is required to tighten and hold the quadriceps muscle on the top of the thigh without actually moving the knee itself. Gradually though, the strengthening exercises will be advanced and will address any individual deficits in strength that your Physical Therapist has identified around the knee, and hip area, which controls the knee position. Eccentric exercises, as explained above under non-surgical treament, will also eventually be added in order to prepare your child’s knee for the rigorous bending involved in both everyday and sporting activities.
As a final component to your child’s rehabilitation, your therapist will also prescribe proprioceptive exercises. These exercises help to improve the ability of the joint to know where it is in space and encourage the muscles to work together to control the knee joint. As with all rehabilitation exercises, your therapist will closely monitor the technique used and the alignment of your child’s knee as they do the exercises in order to ensure that they are not compensating in any way, which can lead to ongoing pain or a secondary injury.
When you’re child is well under way with their rehabilitation, regular visits to Peak Physical Therapy will end. Your Physical Therapist will continue to be a resource, but with your supervision, your child will be in charge of doing their exercises as part of an ongoing home program. Generally rehabilitation at Peak Physical Therapy after surgery for Osgood Schlatter Disease goes extremely well and children can eventually return without difficulties to the activities they enjoy participating in. If, however, your child’s pain is lasting longer that your therapist thinks it should or your child is not progressing as rapidly as your therapist would expect, they will ask you to follow up with your child’s surgeon to ensure that there are no complicating factors from the surgery that are impeding rehabilitation.
Portions of this document copyright MMG, LLC.
 An Osgood-Schlatter lesion involves pain and swelling in the small boney bump on the front of the tibia (shinbone), right below the kneecap. It primarily occurs in children and adolescents. The problem affects the area where bone growth occurs. Too much stress on the growing bone causes the pain and swelling. The pain often worsens with activity and eases with rest. Fortunately, the condition is not serious and it is usually only temporary.
An Osgood-Schlatter lesion involves pain and swelling in the small boney bump on the front of the tibia (shinbone), right below the kneecap. It primarily occurs in children and adolescents. The problem affects the area where bone growth occurs. Too much stress on the growing bone causes the pain and swelling. The pain often worsens with activity and eases with rest. Fortunately, the condition is not serious and it is usually only temporary.











 Osgood-Schlatter lesions fit into a category of bone development disorders known as osteochondroses. (Osteo means bone, and chondro means cartilage.) In normal development, specialized bone growth centers (called growth plates) change over time from cartilage to bone. The growth centers expand and finally unite. This is how bones grow in length and width. Bone growth centers are located throughout the body.
Osgood-Schlatter lesions fit into a category of bone development disorders known as osteochondroses. (Osteo means bone, and chondro means cartilage.) In normal development, specialized bone growth centers (called growth plates) change over time from cartilage to bone. The growth centers expand and finally unite. This is how bones grow in length and width. Bone growth centers are located throughout the body.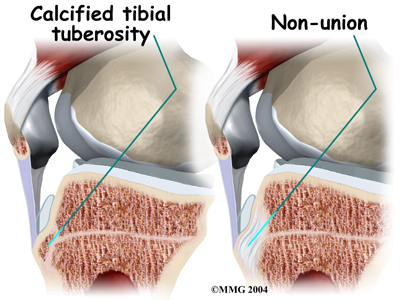 In an Osgood-Schlatter lesion, the tibial tuberosity is often enlarged and painful. It hurts when bumped. It also hurts when pressure is put on it, such as when kneeling. Activities like running, jumping, climbing, and kicking may hurt because of the tension of the patellar tendon pulling on the tibial tuberosity.
In an Osgood-Schlatter lesion, the tibial tuberosity is often enlarged and painful. It hurts when bumped. It also hurts when pressure is put on it, such as when kneeling. Activities like running, jumping, climbing, and kicking may hurt because of the tension of the patellar tendon pulling on the tibial tuberosity.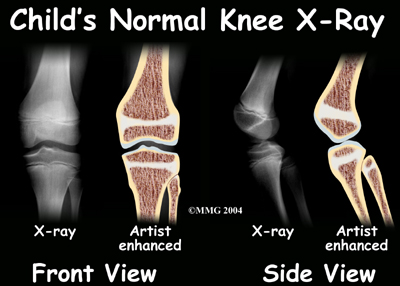 Next your Physical Therapist will do a physical examination of both your child’s painful and non-painful knee, and examine the entire lower extremities for factors contributing to the problem. Your therapist will palpate, or touch, around the knee and particularly along the patellar tendon and at the tibial tuberosity to determine the exact location of pain and to note any swelling. They will assess the stability of the knee joint to determine if the laxity of the ligaments and tissues surrounding the knee joint are contributing to the problem.
Next your Physical Therapist will do a physical examination of both your child’s painful and non-painful knee, and examine the entire lower extremities for factors contributing to the problem. Your therapist will palpate, or touch, around the knee and particularly along the patellar tendon and at the tibial tuberosity to determine the exact location of pain and to note any swelling. They will assess the stability of the knee joint to determine if the laxity of the ligaments and tissues surrounding the knee joint are contributing to the problem.  Your doctor may prescribe anti-inflammatory medicine to help reduce swelling.
Your doctor may prescribe anti-inflammatory medicine to help reduce swelling. In some cases, your child may need to stop sporting activities for a short period, which allows the pain and inflammation to calm down. If the bone has completely separated then it is necessary to completely avoid sports. Fortunately it is not common that the bone completely separates, so not all athletes need to entirely avoid sports. Patients who do require a rest usually don't need to avoid sports for a long time, and often a relative rest is adequate. Taking a relative rest means decreasing the intensity or frequency of certain activities but not eliminating them completely. Your Physical Therapist will advise you regarding whether or not your child needs to cease or decrease their activity. Pain that is intense enough to continue during the night, is constant, causes a limp while walking, or needs to be regularly relieved with over the counter pain medication is considered severe enough that activities need to be ceased for a defined period of time. In only very severe cases is bracing or casting recommended for periods of up to 6 weeks in order to give the chance for the pain and inflammation in the knee to calm down.
In some cases, your child may need to stop sporting activities for a short period, which allows the pain and inflammation to calm down. If the bone has completely separated then it is necessary to completely avoid sports. Fortunately it is not common that the bone completely separates, so not all athletes need to entirely avoid sports. Patients who do require a rest usually don't need to avoid sports for a long time, and often a relative rest is adequate. Taking a relative rest means decreasing the intensity or frequency of certain activities but not eliminating them completely. Your Physical Therapist will advise you regarding whether or not your child needs to cease or decrease their activity. Pain that is intense enough to continue during the night, is constant, causes a limp while walking, or needs to be regularly relieved with over the counter pain medication is considered severe enough that activities need to be ceased for a defined period of time. In only very severe cases is bracing or casting recommended for periods of up to 6 weeks in order to give the chance for the pain and inflammation in the knee to calm down.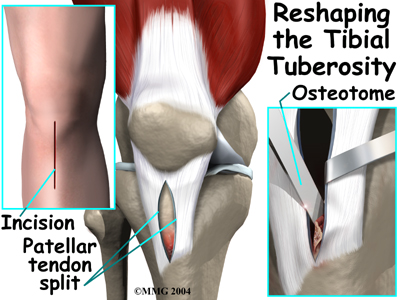 Surgery is not considered for an Osgood-Schlatter lesion unless bone growth is complete and symptoms are still bothersome despite nonsurgical treatments. Even under these circumstances, surgery is rarely recommended.
Surgery is not considered for an Osgood-Schlatter lesion unless bone growth is complete and symptoms are still bothersome despite nonsurgical treatments. Even under these circumstances, surgery is rarely recommended.


